Fentanyl crisis in WA needs a turning point, so what is being done?
SEATTLE — Washington came to understand the scope and severity of the state's fentanyl crisis in 2023 more than any other year.
Statistics have gone from bad to worse:
Fentanyl set a record of fatal overdoses in 2023, with 1,082 — a 51% increase over record-setting 2022.
In September, five members of the Lummi Nation died in one week, a particularly high toll for the tribe, which has been disproportionately hit by the opioid crisis.
The Seattle Fire Department averaged about 15 overdose calls a day in 2023, surpassing last year's total by early fall.
University of Washington researchers are at work on a study that, in preliminary analyses, suggests opioid use disorder happens "way faster with fentanyl than it does with heroin," said Caleb Banta-Green, director for the UW Community-Engaged Drug Education, Epidemiology and Research.
"The point is," he said, "there's no time to wait."
Across the state, people who experience and see the effects of the drug are watching to see if officials act with that sense of urgency.
State lawmakers made fentanyl one of the pressing issues in the short legislative session. A new Seattle City Council has also named the drug crisis a top priority, inspiring a renewed focus on law and order. King County residents await promised treatment options from a recently passed levy and from the Seattle mayor to come to fruition.
On Monday, King County is expected to announce the opening of a new clinic to treat substance use and mental health disorders, as well as an expansion of naloxone kit distribution and an increased number of mobile crisis and outreach teams.
Here are five things to look for in 2024, according to experts from state and local policy, health, education and law enforcement.
1. A rising tide of pills — and overdoses
Overdose numbers in the past few years have been "staggering," Banta-Green said, and will have to peak at some point — though he's not sure it will be this year.
"It's hard to imagine we'd be still increasing at the rate we've been going at," Banta-Green said. "You'd think it would slow down. But I don't think it's going to slow because of improved services; I think it's going to slow because people are dying."
Based on what Seattle police are seeing on the streets, police Chief Adrian Diaz said he won't be surprised if 2024 ends with another 1,000 overdose deaths countywide from the synthetic opioid, given the drug's broadening availability, declining cost and growing potency.
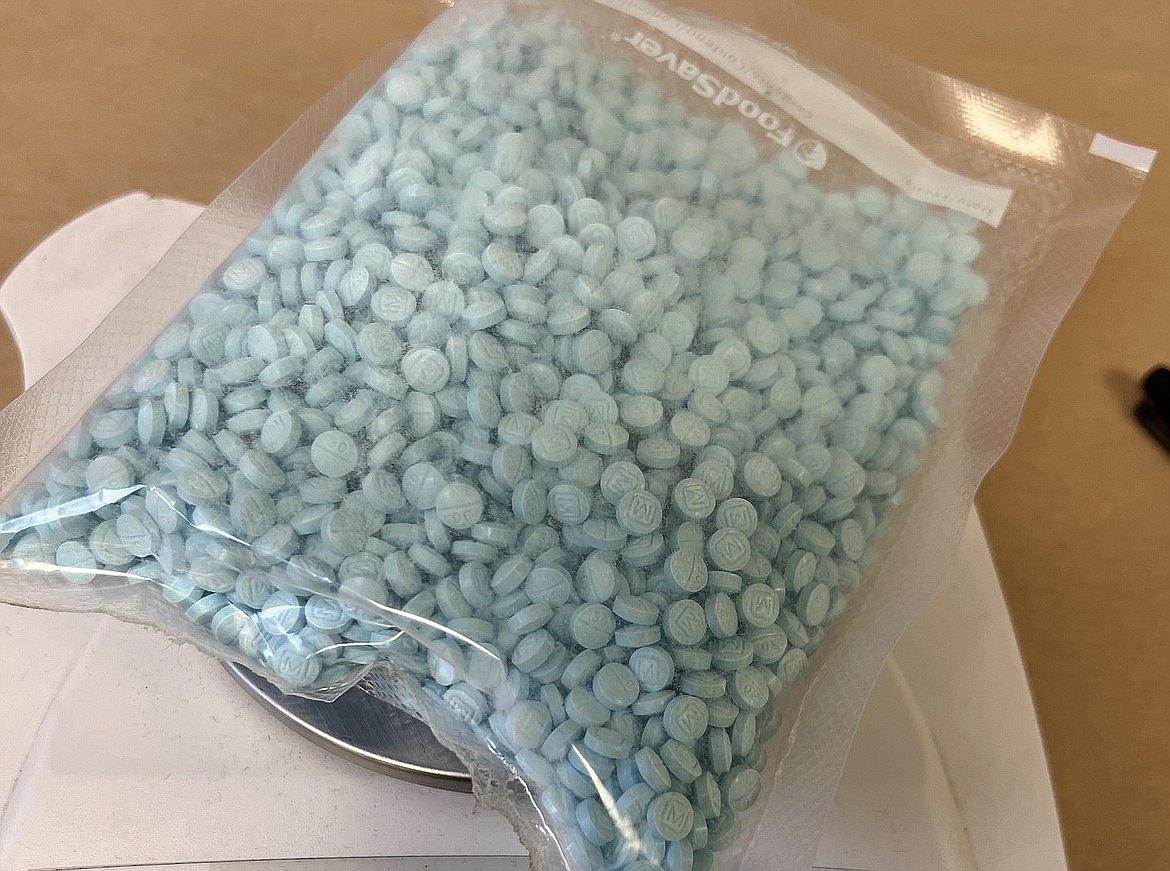
Five years ago, when fake M30 pills laced with fentanyl first started showing up in the local drug supply, the blue pills sold for $15 apiece, Diaz said. By fall 2022, the price had fallen to $2 or $3 per pill. Now, it costs about $1 per pill — an indication of just how much fentanyl is being smuggled into the area, he said.
"What it costs right now shows us that we still have a huge concern that all of our agencies need to be working on," Diaz said.
The Seattle Police Department, both on its own and in joint operations with other local and federal agencies, seized a total of 2 million fentanyl pills last year, Diaz said. While lethal doses used to be found in 2 or 3 out of every 10 pills seized, he said 7 out of 10 pills now being seized contain enough fentanyl to trigger a fatal overdose.
2. ERs become increasingly taxed
Health care and hospital leaders think pressure on emergency rooms will worsen without more accessible treatment options for poor and homeless people.
They say that many of the region's emergency rooms have become a "social safety net for unhoused residents."
In Washington, about 1 in 10 ER visits are by people experiencing homelessness, the majority of whom seek care for a substance-use disorder alone or in combination with a mental health condition, according to a report from the Washington State Hospital Association and Challenge Seattle, a consortium of the region's business leaders.
The report called for more street medicine teams and low-barrier, 24/7 sites where people can stabilize and receive treatment. It also recommended accelerating the development of new behavioral health facilities with a focus on the fentanyl crisis and securing more sustainable funding for these efforts.
Without a renewed push for efforts like these, state hospital leaders predict worse patient care, higher health care costs, capacity issues and staff burnout.
Availability of Brixadi, a new long-acting injectable medication for opioid use disorder, could smooth treatment for those living outside and for those who are still weighing their treatment options, said Dr. Nathan Kittle, addiction medicine specialty director at Healthpoint, a nonprofit network of community health centers.
Until recently, a monthly injection called Sublocade was the only available long-acting medication meant to curb withdrawals and reduce opioid cravings. Brixadi, which can be administered weekly, gives patients a chance to try out medication without committing to a monthlong dose, Kittle said. The U.S. Food and Drug Administration approved the medication last spring.
Unlike Sublocade, he added, Brixadi doesn't have to be refrigerated. This could make it easier for mobile health care workers to deliver the shot to people who are unhoused, he said.
3. A fight over ownership of the problem
Seattle Mayor Bruce Harrell issued a fentanyl executive order last year, which included promises that could help reduce the number of fatal overdoses and lead more people to seek long-term addiction care.
At his state of the city address, he announced $7 million for a "post-overdose" facility that would provide treatment and casework. He also said he would establish a work group to better understand the intersection of the criminal legal system and substance use, as well as launch a program offering financial incentives to people struggling with addiction. Some are underway.
While the city pays into the region's public health body, Harrell has repeatedly said in recent months that substance use treatment and strategy is under the purview of the county.
"That's a critical distinction," he said.
Both council President Sara Nelson and Harrell have called for a review of how city dollars are being spent in the joint effort of Public Health — Seattle & King County.
Much of the new Seattle City Council made fighting the fentanyl crisis central to their campaigns.
Nelson called for approaches beyond mobile response teams and anti-addiction medication.
"That's what we've been doing for years," she said. "This is a new drug and a new crisis and there's an explosion of overdose deaths, so we can't just keep doing that, we have to expand our toolbox."
4. More enforcement but maybe not more jail
The city says more police and jail involvement for fentanyl users could be coming.
Nelson said an arrest is "a chance for people to sober up for a little bit and consider a different path" and can wear people down to accept treatment.
Diaz and the Seattle City Attorney's Office are in talks to potentially create a threshold of how many times a person can overdose and refuse treatment before it becomes a bookable offense. He said officers are seeing the same people multiple times a day, and he wants a way to get them to accept treatment.
Jail might not be an option for most people arrested, though.
Although the city ordinance passed in October allows officers to make arrests for gross misdemeanor drug possession, that charge alone won't land someone in jail. The understaffed King County Jail has restricted intakes to felonies and misdemeanors involving guns, stalking, alcohol-related driving and domestic violence.
Of the 174 people arrested for gross misdemeanor drug possession or public use since the city ordinance went into effect, 96 have been referred to a diversion program, and a couple dozen more were booked into jail either on warrants or after committing new offenses, according to Diaz.
Officers have referred more than 30 cases to the City Attorney's Office for a charging decision, 13 people were identified and released at the scene, and four were turned away from the jail due to health issues.
Enforcement of the law has also been scaled back since its start.
About 20 people have been arrested in targeted enforcement each week, though police have prioritized gun violence, overall crime and weekly protests over the ongoing war in Gaza. The weekly operations are expected to continue, but their reach depends on staffing.
5. Better treatment and outreach to youth
Washington high schools are likely better equipped to prevent opioid overdoses in 2024, some experts say, now that the state is kicking in new prevention resources.
School districts with 2,000 or more students are already required by law to stock the opioid-reversal drug naloxone. In January, the state's health department said it planned to make it easier for schools to get the medication by offering two free intranasal naloxone kits to any public high school that wanted them.
"That's one step to hopefully prevent unnecessary deaths," said Kittle.
Spreading awareness about opioid use disorder in youth — and medications to treat it — will continue to be a major priority in 2024, said Banta-Green. "I don't know the quality of those [awareness] campaigns. I don't know what the messages are. I don't know if they're going to be effective. But I believe there'll be growing awareness."
A bill that passed both chambers last week will, if signed by Gov. Jay Inslee, require schools to provide education about fentanyl and other opioids in health classes to as many seventh- and ninth-grade students as possible during the remainder of the 2024-25 school year. After that, seventh and ninth graders would get the training every year.
"Because if they're not safe, they don't learn, and don't get the education that they need," said Sen. Lisa Wellman, D-Mercer Island, sponsor of the bill.
Three times as many kids and teens died from an opioid-related overdose in 2022 than did in 2019, state data shows. It's tough to predict whether that upward trend will continue, but "from no one am I hearing that things are getting better," Banta-Green said.
Seattle Times staff reporters David Kroman, Sara Jean Green, Hannah Furfaro, Elise Takahama, Jacquelyn Jimenez Romero and Claire Bryan contributed to this report.